Lyme Disease
What Is Lyme Disease?
Lyme disease is the leading tick-borne disease in the United States. It's most common in the Northeast and the northern midwestern states.
Lyme disease is caused by a type of found in animals like mice and deer. Deer ticks (also called black-legged ticks) that feed on these animals can then spread the bacteria to people through tick bites.
You probably won't see it happening. Deer ticks are tiny, so it's very hard to see them. Immature ticks (called "nymphs") are about the size of a poppy seed. Adult ticks are about the size of a sesame seed.
It's easy to overlook a tick bite. Many people who get Lyme disease don't remember being bitten. The good news is that most tick bites don't lead to Lyme disease. But it still helps to know what to watch for.
What Are the Signs & Symptoms of Lyme Disease?
Some people don’t have any symptoms at all when they get infected. When symptoms do happen, they can vary from person to person and often happen in three stages:
Two Early Stages
For the first few weeks, symptoms may include:
- a rash at the site of the tick bite, which usually is round or oval. Some rashes have a clear middle (called a bulls-eye rash).
- fever
- tiredness
- headache
- muscle aches
- joint pain

If not treated, the infection can spread to other areas and cause:
- rashes on parts of the body not near the tick bite
- slow or irregular heartbeat
- problems with the nervous system (brain and spinal cord) including:
- damage to a facial nerve that can cause drooping (facial palsy)
- numbness in arms or legs
- mood changes
- memory problems
- neck stiffness and pain due to inflammation of the brain and spinal cord (meningitis)
Late Stage
If Lyme disease goes untreated for months, the earlier symptoms can continue. The person also can develop arthritis (a red, swollen, painful joint).
This wide range of symptoms can make Lyme disease hard for doctors to diagnose. But they can order blood tests to look for signs of the body's reaction to Lyme disease.
When Should I Call the Doctor?
If a tick bites you, call your doctor. Other conditions can cause similar symptoms, so it's always a good idea to discuss them with your doctor. That way you can get checked and treated, if needed. Call right away if you get a red-ringed rash, lasting flu-like symptoms, joint pain or a swollen joint, or facial paralysis.
How Is Lyme Disease Treated?
Doctors usually treat Lyme disease with a 2- to 4-week course of antibiotics. People whose Lyme disease is diagnosed quickly and treated with antibiotics almost always have a good outcome. They usually feel back to normal within several weeks of starting treatment.
Is Lyme Disease Contagious?
Lyme disease is not contagious, so you can't catch it from another person. But you can get it more than once from ticks that live on deer, in the woods, or travel on your pets. So always be cautious, even if you've already had Lyme disease.
Can Lyme Disease Be Prevented?
There's no sure way to avoid getting Lyme disease. But you can minimize your risk. Be aware of ticks when you're in high-risk areas. If you work outdoors or spend time gardening, fishing, hunting, or camping, take precautions:
- Wear closed shoes or boots, long-sleeved shirts, and long pants. Tuck your pant legs into your shoes or boots to prevent ticks from crawling up your legs.
- Use an insect repellent containing 10% to 30% DEET (N,N-diethyl-meta-toluamide).
- Wear light-colored clothing to help you see ticks more easily.
- Keep long hair pulled back or wear a hat for protection.
- Don't sit on the ground outside.
- Check yourself for ticks regularly — both indoors and outdoors. Wash your clothes and hair after leaving tick-infested areas.
If you use an insect repellent containing DEET, follow the directions on the product's label and don't overapply it. Place DEET on shirt collars and sleeves and pant cuffs, and only use it directly on exposed areas of skin. Be sure to wash it off when you go back indoors.
No vaccine for Lyme disease is currently on the market in the United States.
How Do I Remove a Tick?
You should know how to remove a tick just in case one lands on you or a friend. To be safe, remove the tick as soon as possible.
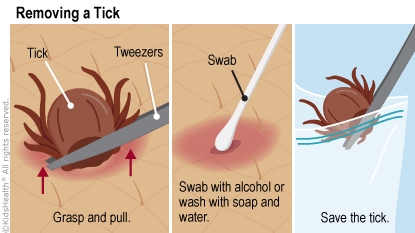
If you find a tick:
- Call your doctor, who may want you to save the tick after removal so that the tick can later be identified as the type that may carry Lyme disease. You can put the tick in a sealed container to preserve it.
- Use tweezers to grasp the tick firmly at its head or mouth, next to your skin.
- Pull firmly and steadily on the tick until it lets go of the skin. If part of the tick stays in your skin, don't worry. It will eventually come out. But call your doctor if you notice any irritation in the area or symptoms of Lyme disease.
- Swab the bite site with alcohol.
Note: Don't use petroleum jelly or a lit match to kill a tick. They won't get the tick off your skin quickly enough, and may just cause it to burrow deeper into your skin.
