Osteogenesis Imperfecta (Brittle Bone Disease)
What Is Osteogenesis Imperfecta?
Osteogenesis imperfecta (OI) is a genetic disorder that prevents the body from building strong bones. That’s why it’s also called brittle bone disease.
There are different types of OI, and the problems it causes vary. Some people have mild symptoms, like bones that break a little easier than normal. Others can have serious problems. Treatments can help people with osteogenesis imperfecta reach their full potential.
What Causes Osteogenesis Imperfecta?
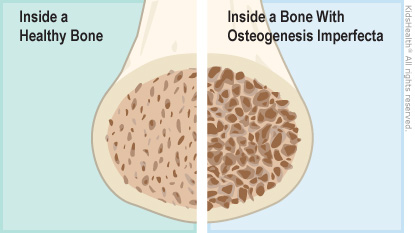
Osteogenesis imperfecta (os-tee-oh-JEN-uh-sis im-pur-FEK-tuh) happens because of a mutation (change) in the gene that makes the protein collagen. Collagen is an important building block of bones.
Children may inherit the mutation from a parent. Sometimes, though, it is not inherited and neither parent has osteogenesis imperfecta. Instead, the change happens early in pregnancy when the baby is first forming.
People who have brittle bone disease are born with it. They either don't have enough collagen in their bones or the collagen doesn't work as it should. This makes their bones weaker and more brittle than normal bones. It also can lead to abnormally shaped bones.
What Are the Signs & Symptoms of Osteogenesis Imperfecta (OI)?
Symptoms of the condition vary from person to person. Even people from the same family, or with the same type of OI, can have different symptoms.
The most common types of osteogenesis imperfecta and their usual symptoms are:
Type I: This is the mildest and most common type of brittle bone disease. The collagen is normal, but there isn’t enough of it. People with type I have bones that break more easily, but their bones are usually shaped normally. The first bone break usually happens when the child starts walking. Fractures usually happen less often after puberty. The whites of the eyes (sclera) can have a blueish tint. They may also have hearing loss as adults.
Type II: This is the most severe type. The collagen is not formed normally. Babies with type II are usually born with many fractures, are very small, and have severe breathing problems. As a result, most do not survive.
Type III: In this type, collagen doesn’t form normally, and babies often have broken bones at birth. As kids get older, their bones can break easily, and they’re usually shorter than other kids their age. They may have abnormally shaped bones (such as a curved spine, a ribcage that points outward, a triangular face, or legs that bow out), breathing problems (which can be life-threatening), hearing loss as adults, brittle teeth, and other problems. The whites of their eyes can have a blueish tint.
Type IV: Collagen also doesn’t form normally in type IV. Kids usually have frequent bone breaks (which may happen less often after puberty) and abnormally shaped bones (similar to type III). They’re shorter than other kids their age and may have hearing loss as an adult.
How Is Osteogenesis Imperfecta (OI) Diagnosed?
If someone has a family member with osteogenesis imperfecta, doctors can do tests to see if a child has it. Before a baby is born, they can order a prenatal ultrasound to check for any broken or unusually shaped bones or an amniocentesis to check for mutations in the collagen gene.
If OI is not diagnosed before birth, doctors can do tests after a baby is born. They also might order tests when there is no family history of OI if:
- a child has frequent or unexplained bone fractures, dental problems, blue sclera, or short stature
- a prenatal ultrasound shows broken or abnormally shaped bones
To test for osteogenesis imperfecta in babies and children, doctors may order:
- X-rays, which can show fractures or healed breaks
- genetic tests, to look for the collagen gene mutation
- biochemical testing, which may include a skin sample to examine the collagen
How Is Osteogenesis Imperfecta (OI) Treated?
There's no cure for osteogenesis imperfecta. But a care team can help kids with problems related to the condition.
If your child has brittle bone disease, the care team can include:
- a primary care provider (for routine health care)
- an orthopedic surgeon (for bone problems)
- a physical therapist (to help with strength and movement)
- an occupational therapist (to help with doing everyday activities)
- a pulmonologist (to help with any breathing problems)
Treatment can include:
- medicines to strengthen bones and lower their chances of breaking
- preventing broken bones by avoiding activities that may lead to falls (such as skiing) or put too much stress on the bones (such as jumping on a trampoline)
- getting treatment from an orthopedic surgeon right away when bones do break
- doing low-impact exercises (such as swimming) to help build muscle strength and increase bone strength
- physical therapy (PT) to build muscle strength, build overall fitness, and improve breathing. PT can help kids learn to use mobility aids, if needed.
- occupational therapy (OT) to help kids learn to use assistive devices, if needed. In younger kids, it can help with motor skill development.
- surgery to fix a broken or abnormally shaped bone. Surgeons also might put a metal rod into the thighbone or arm bone to prevent broken bones.
- surgery for hearing problems
- treatment for dental problems
How Can Parents Help?
With your support, your child can get the medical care they need to live their healthiest life. Be sure to:
- Schedule and go to all needed medical care and therapy visits.
- Follow the care team’s recommendations on giving medicines.
- Help your child find activities and hobbies that are safe and enjoyable. Check with your doctor about any sports to avoid. Music, art, computers, writing, or photography are all great options.
- Help your child learn about brittle bone disease and their possible health care needs as they get older and more independent.
- Stay active together as a family. Choose activities that your child can do.
Having a child with a lifelong illness can be stressful. You can find support and more information through the care team and online at:
