- Parents Home
- Para Padres
- A to Z Dictionary
- Allergy Center
- Asthma
- Cancer
- Diabetes
- Diseases & Conditions
- Doctors & Hospitals
- Emotions & Behavior
- First Aid & Safety
- Flu (Influenza)
- Food Allergies
- General Health
- Growth & Development
- Heart Health & Conditions
- Homework Help Center
- Infections
- Newborn Care
- Nutrition & Fitness
- Play & Learn
- Pregnancy Center
- Preventing Premature Birth
- Q&A
- School & Family Life
- Sports Medicine
- Teens Home
- Para Adolescentes
- Asthma
- Be Your Best Self
- Body & Skin Care
- Cancer
- Diabetes
- Diseases & Conditions
- Drugs & Alcohol
- Flu (Influenza)
- Homework Help
- Infections
- Managing Your Weight
- Medical Care 101
- Mental Health
- Nutrition & Fitness
- Q&A
- Safety & First Aid
- School, Jobs, & Friends
- Sexual Health
- Sports Medicine
- Stress & Coping
Myelomeningocele
What Is Myelomeningocele?
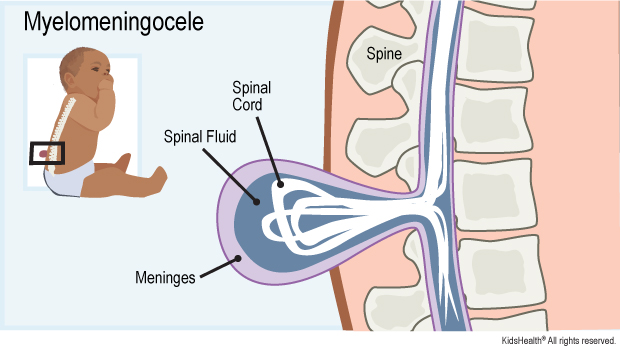
Myelomeningocele (my-uh-lo-meh-NIN-guh-seal) is a type of spina bifida. Spina bifida (SPY-nuh BIF-ih-duh) happens when a baby's backbone (spine) does not form normally during pregnancy. The baby is born with a gap in the bones of the spine.
A myelomeningocele is a sac that contains:
- part of the spinal cord
- its covering (called the meninges)
- spinal fluid
It pushes through the gap in the spine and the skin. It can be seen on the baby's back.
What Are the Signs & Symptoms of a Myelomeningocele?
The signs and symptoms of a myelomeningocele depend on where it is. A myelomeningocele can lead to:
- weakness, loss of feeling, or trouble moving body parts below the level of the myelomeningocele
- problems with bladder (pee) and bowel (poop) control
- too much spinal fluid in the brain (hydrocephalus)
- problem with how the brain is formed (Chiari malformation)
- learning problems
- seizures
Sometimes babies with a myelomeningocele are born with other medical problems like clubfoot, curvature of the spine, hip problems, heart problems, or kidney problems.
What Are the Other Types of Spina Bifida?
Other kinds of spina bifida include:
- Spina bifida occulta: This is a gap in the bones in the spine but the spinal cord and meninges do not push through it. They are in their normal place inside the spinal canal, and there's no opening on the baby's back.
- Meningocele: This is when a sac that contains spinal fluid pushes through the gap in the spine. The spinal cord is in its normal place in the spinal canal. The skin over the meningocele often is open.
What Causes a Myelomeningocele?
All types of spina bifida happen in the first month of pregnancy. At first, a fetus' spinal cord is flat. It then closes into a tube called a neural tube. If this tube does not fully close, the baby is born with spina bifida. In myelomeningocele, a sac containing part of the spinal cord, meninges, and spinal fluid push through the gap in the spine and the skin.
It's not clear why some babies get a myelomeningocele. It can happen if a woman does not get enough of the vitamin folic acid early in her pregnancy. A woman also might be more likely to have a baby with a myelomeningocele if she:
- takes some types of seizure medicines during pregnancy
- already has had a baby with spina bifida
- has diabetes
How Is Myelomeningocele Diagnosed?
During pregnancy, a blood test called alpha-fetoprotein (AFP) can tell if a woman has a higher risk of having a baby with a myelomeningocele. A prenatal ultrasound or fetal MRI also can show whether a baby has one.
A myelomeningocele that's not diagnosed during pregnancy is seen when the baby is born.
How Is Myelomeningocele Treated?
After delivery, a baby born with a myelomeningocele will need:
- surgery to close the skin over the myelomeningocele (usually within 3 days)
- testing for Chiari malformation and hydrocephalus with an ultrasound, CT scan, or MRI
- regular checks of head size to see if hydrocephalus develops
- regular checks of movements to see how the spinal cord and nerves are working
Other medical care will depend on a child's needs. Treatments can include:
- a shunt for hydrocephalus (the shunt drains the spinal fluid into the belly so it doesn't build up in the spaces in the brain)
- leg braces to help with walking
- a wheelchair
- a tube (called a catheter) to help empty the bladder
- surgery on the spine or legs
- surgery for Chiari malformations
- physical therapy (PT)
- occupational therapy (OT)
- special help at school
Some myelomeningoceles found before birth are treated with surgery while the baby is still in the womb. Sometimes this can lower the chances of the baby getting hydrocephalus later. And it might increase the strength of the child's legs. There are risks to the mom and baby from this surgery, so doctors and families have to decide together if the surgery is right for them.
How Can Parents Help?
Most children with myelomeningocele will need ongoing medical care. To help your child stay as healthy as possible:
- Take your child to all medical care visits.
- Follow all treatment recommendations, such as giving medicines and going to PT and OT.
Call your doctor right away if your child has:
- new weakness
- worsening bladder or bowel control
- headaches
- vomiting
- tiredness
- back pain or pain at the myelomeningocele site
- neck pain, trouble swallowing, or voice changes
What Else Should I Know?
Having a child with a serious medical condition can feel overwhelming for any family. But you're not alone, and many resources are available to help you and your family. Talk to anyone on the care team about ways to find support. You also can find more information online at:

© 1995- The Nemours Foundation. KidsHealth® is a registered trademark of The Nemours Foundation. All rights reserved.
Images sourced by The Nemours Foundation and Getty Images.