- Parents Home
- Para Padres
- A to Z Dictionary
- Allergy Center
- Asthma
- Cancer
- Diabetes
- Diseases & Conditions
- Doctors & Hospitals
- Emotions & Behavior
- First Aid & Safety
- Flu (Influenza)
- Food Allergies
- General Health
- Growth & Development
- Heart Health & Conditions
- Homework Help Center
- Infections
- Newborn Care
- Nutrition & Fitness
- Play & Learn
- Pregnancy Center
- Preventing Premature Birth
- Q&A
- School & Family Life
- Sports Medicine
- Teens Home
- Para Adolescentes
- Asthma
- Be Your Best Self
- Body & Skin Care
- Cancer
- Diabetes
- Diseases & Conditions
- Drugs & Alcohol
- Flu (Influenza)
- Homework Help
- Infections
- Managing Your Weight
- Medical Care 101
- Mental Health
- Nutrition & Fitness
- Q&A
- Safety & First Aid
- School, Jobs, & Friends
- Sexual Health
- Sports Medicine
- Stress & Coping
Developmental Dysplasia of the Hip
What Is Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip (DDH) is a problem with the way a baby's hip joint forms. Sometimes the condition starts before the baby is born, and sometimes it happens after birth, as the child grows. It can affect one hip or both.
Most infants treated for DDH develop into active, healthy kids and have no hip problems.
What Happens in a Hip With Developmental Dysplasia?
The hip joint is a ball and socket joint. The top part of the thighbone (the ball part of the hip) sits inside a socket that's part of the pelvic bone. The ball moves around in different directions, but always stays inside the socket. This lets us move our hips front, back, and side to side. It also supports our body weight for walking and running.
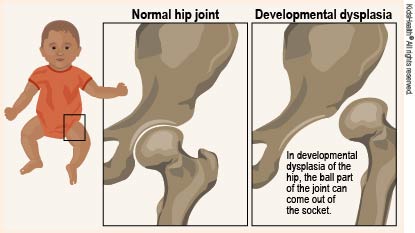
In DDH, the hip does not form well. The ball part of the joint may be completely, or partly, out of the socket. Sometimes the ball part may slide in and out of the socket. Often, the socket is shallow. If this is not fixed, the hip joint will not grow well. This can lead to pain with walking and hip arthritis at a young age.
What Are the Signs & Symptoms of Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip doesn't cause pain in babies, so can be hard to notice. Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Parents could notice:
- The baby's hips make a popping or clicking that is heard or felt.
- The baby's legs are not the same length.
- One hip or leg doesn't move the same as the other side.
- The skin folds under the buttocks or on the thighs don't line up.
- The child has a limp when starting to walk.
Babies with any of these signs should see a doctor to have their hips checked. Finding and treating DDH early usually means there's a better chance for a baby's hips to develop normally.
What Is Hip Laxity?
Many babies are born with hips that feel loose when moved around. This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
A baby's whose hip ligaments are still loose after 6 weeks might need treatment. So follow-up doctor visits for babies with hip laxity are important.
Who Gets Developmental Dysplasia of the Hip?
Any baby can have DDH. But there's a higher chance of being born with it in babies who:
- are girls
- are first-born
- were breech babies (in the womb buttocks-down instead of head-down), especially during the third trimester of pregnancy
- have a family member with the condition, such as parent or sibling
Rarely, a baby isn't born with DDH, but develops it after birth. To prevent DDH in babies who aren't born with it, don't swaddle a newborn's hips or legs tightly together. Always make sure a baby's legs have plenty of wiggle room.
How Is Developmental Dysplasia of the Hip Diagnosed?
Doctors find most cases of DDH during well-child exams. If a baby has signs of DDH or has a higher risk for it, the doctor will order tests.
Two tests help doctors check for DDH:
- An ultrasound uses sound waves to make pictures of the baby's hip joint. This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray.
- An X-ray works best in babies older than 4–6 months. At that age, their bones have formed enough to see them on an X-ray.
How Is Developmental Dysplasia of the Hip Treated?
A pediatric orthopedic surgeon (a specialist in children's bone conditions) cares for babies and kids with DDH. The goal of care is to get the ball of the hip in the socket and keep it there, so the joint can grow normally.
The orthopedic surgeon chooses the treatment based on the child's age. Options include:
- bracing
- a closed reduction and casting
- an open reduction (surgery) and casting
A brace or cast will hold the hip in place and will be on both sides, even if only one hip is affected.
Bracing
Treatment for babies younger than 6 months old usually is a brace. The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
Treatment with the Pavlik harness often lasts about 6–12 weeks. While wearing the harness, the baby has a checkup every 1–3 weeks with hip ultrasounds and exams. During the visit, the medical team can adjust the harness if needed.
The harness (brace) usually works well to keep the hips in position. Most babies won't need other treatment.
Rarely, the harness isn't able to keep the ball of the hip in the socket. Then, doctors might do either:
- a closed reduction (manually moving the ball back into the socket) and casting
- an open reduction (surgery) and casting
Closed Reduction and Casting
A child might need a closed reduction if:
- The harness was not successful at keeping the ball of the hip in the socket.
- A baby starts care after age 6 months.
For a closed reduction, the baby gets medicine (general anesthesia) to sleep through the procedure and not feel pain. The surgeon:
- Injects contrast dye into the joint to see the part of the ball.
- Moves the baby's thighbone so that the ball of the joint goes back into place in the socket.
- Puts on a hip spica cast to hold the hip in place. The baby wears the cast for 2–4 months.
Sometimes, the orthopedic surgeon also loosens the tight muscle in the groin during the closed reduction.
Open Reduction (Surgery) and Casting
A child might need surgery (an open reduction) if:
- The closed reduction was not successful at keeping the ball of the hip in the socket.
- The child is older than 18 months when starting treatment.
During an open reduction, the child is asleep under anesthesia. The surgeon:
- Makes a cut through the skin.
- Moves muscles out of the way to see the hip joint directly.
- Puts the ball back into place.
- Closes the surgical cut with stitches placed under the skin. These won't need to be removed.
- Puts on a hip spica cast to hold the hip in place. The child wears the cast for 6–12 weeks.
Sometimes, the orthopedic surgeon also does a surgery on the pelvic bone to deepen a very shallow hip socket, especially for a child older than 18 months.
What Else Should I Know?
Kids will have regular checkups with their orthopedic specialist until they're 16–18 years old and done growing. These help make sure the hip develops well.

© 1995- The Nemours Foundation. KidsHealth® is a registered trademark of The Nemours Foundation. All rights reserved.
Images sourced by The Nemours Foundation and Getty Images.