- Home
- Humana Medicaid
- Kentucky Medicaid
- Medicaid extras
- Health and wellness
- Parents Home
- Para Padres
- A to Z Dictionary
- Allergy Center
- Asthma
- Cancer
- Diabetes
- Diseases & Conditions
- Doctors & Hospitals
- Emotions & Behavior
- First Aid & Safety
- Flu (Influenza)
- Food Allergies
- General Health
- Growth & Development
- Heart Health & Conditions
- Homework Help Center
- Infections
- Newborn Care
- Nutrition & Fitness
- Play & Learn
- Pregnancy Center
- Preventing Premature Birth
- Q&A
- School & Family Life
- Sports Medicine
- Teens Home
- Para Adolescentes
- Asthma
- Be Your Best Self
- Body & Skin Care
- Cancer
- Diabetes
- Diseases & Conditions
- Drugs & Alcohol
- Flu (Influenza)
- Homework Help
- Infections
- Managing Your Weight
- Medical Care 101
- Mental Health
- Nutrition & Fitness
- Q&A
- Safety & First Aid
- School, Jobs, & Friends
- Sexual Health
- Sports Medicine
- Stress & Coping
Tetralogy of Fallot (TOF)
What Is Tetralogy of Fallot (TOF)?
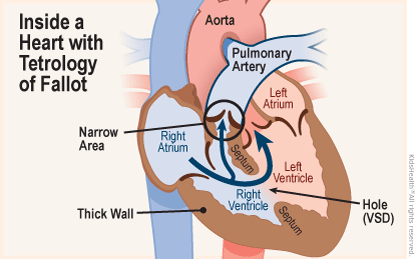
Tetralogy of Fallot (fah-LO) is a congenital (present at birth) heart defect. In tetralogy of Fallot (TOF), four related heart defects change the way blood flows to the lungs and through the heart.
TOF is repaired through open-heart surgery soon after birth or later in infancy. Some infants need more than one heart surgery. Most babies who are treated do very well, but will need regular follow-up visits with a heart specialist.
What Happens in Tetralogy of Fallot (TOF)?
In most cases of tetralogy of Fallot, too little blood goes to the lungs. This low-oxygen (blue) blood then circulates to the rest of the body, and too little oxygen reaches the body tissues.
Babies with TOF often have cyanosis (sy-eh-NO-sis) — a blue or purple tint to the baby's skin, lips, and fingernails.
If tetralogy of Fallot isn't treated, a child may have:
- cyanosis that gets worse
- spells where the blood oxygen levels become very low
- dizziness, fainting, or seizures
- a higher risk of endocarditis, an infection of the inner layer of the heart
- high pressure in the right side of the heart that can cause an irregular heartbeat (an arrhythmia)
Children whose TOF isn't fixed usually become increasingly blue over time and have difficulty participating in physical activities (like playing sports). Most babies who have surgery to correct the defect do very well and can participate in normal kid activities.
How Does Tetralogy of Fallot (TOF) Affect the Heart?
"Tetralogy" means a combination of four related symptoms or problems. The four problems of tetralogy of Fallot are:
- Ventricular septal defect (VSD), which is a hole in the septum, or wall, separating the two lower chambers, or ventricles, of the heart. The septum normally acts as a barrier that prevents blood from both sides of the heart from mixing. But when there is a VSD, the high-oxygen blood from the left ventricle and the low-oxygen blood from the right ventricle can mix. This can lead to either too little or too much blood flow going to the lungs. The VSD in children with TOF is usually large.
- Pulmonary stenosis, a narrowing or thickening of the valve that connects the right ventricle to the pulmonary artery, the blood vessel that carries low-oxygen blood from the heart to the lungs. When in the lungs, blood normally soaks up the oxygen that we breathe and becomes red, oxygen-rich blood. This red blood returns to the heart, and then is pumped to the body.
With pulmonary stenosis, the heart has to work harder than normal to pump blood to the lungs. There is also less blood traveling to the lungs because the pathway is narrowed. This leads to less blood becoming red, oxygen-rich blood. Sometimes, infants with TOF have pulmonary atresia, where the pulmonary valve is completely sealed off. - An "overriding aorta," which means the artery that carries high-oxygen blood to the body is out of place and arises above both ventricles, instead of just the left ventricle, as in a healthy heart. This allows some blood that is low in oxygen to flow into the aorta and out to the body, instead of to the pulmonary artery, which would normally take it to the lungs to pick up oxygen.
- Right ventricular hypertrophy (hi-PER-truh-fee), which is a thickening of the muscular wall of the right ventricle. The thickened wall can contribute to blocking the flow of blood through the pulmonary valve, which allows blood from the heart to flow into the lungs.
What Are the Signs of Tetralogy of Fallot (TOF)?
Cyanosis is a very common sign. Healthy babies can sometimes also have bluish skin around the mouth or eyes from prominent veins under the skin, but their lips and tongue look pink. Babies who have low oxygen levels in the blood usually have blue lips and tongues in addition to bluish skin.
A child with TOF might have sudden episodes of deep cyanosis, called "hypercyanotic spells" or "Tet spells," during crying or feeding. Older children who have Tet spells will often instinctively squat down, which helps to stop the spell.
Other signs include:
- heart murmur
- fussiness
- tiring easily
- trouble breathing
- rapid heartbeat (palpitations)
- fainting
- "clubbing," where the skin or bones around the tips of fingers are widened or rounded (this happens over time in a child with cyanosis)
What Causes Tetralogy of Fallot (TOF)?
The specific cause of tetralogy of Fallot isn't always known. The TOF changes in a baby's heart develop in the early weeks of pregnancy. In some cases, there are genetic causes of TOF — for example, children with Down syndrome or DiGeorge syndrome are more likely to have TOF. Someone born with TOF is more likely to have a child or sibling with it. Each year, roughly 1 out of every 2,500 babies born in the United States have the condition.
Babies of mothers who get rubella (German measles) or other viral illnesses during their pregnancies are at a higher risk for TOF. Other pregnancy-related risks include poor nutrition, alcohol abuse, poorly controlled diabetes, and the mother's age (over 40). Certain environmental factors, such as air pollution, also may increase a mother's chances of having a baby with TOF.
Most of the time, a child with TOF doesn't have any other birth defects.
How Is Tetralogy of Fallot (TOF) Diagnosed?
Doctors might do several tests to find out if a baby has tetralogy of Fallot and to get more details about the baby's heart and blood vessels, including:
- pulse oximeter: a small sensor that clips onto the fingertip, toe, or ear and measures how much oxygen is in the blood. In many newborn nurseries, all babies have a pulse oximeter test before going home to make sure that their oxygen level is normal.
- electrocardiogram (EKG): a test that records the electrical activity of the heart
- echocardiogram (echo): an ultrasound picture of the heart. It records the motion of the blood through the heart and can measure the direction and speed of blood flow.
- chest X-ray
- cardiac catheterization: a thin, flexible tube called a catheter is inserted into the heart, usually through a vein in the leg or arm, and provides information about the heart as well as blood pressure and blood oxygen levels. Sometimes, a device is inserted into the heart or blood vessels through the heart catheter.
- imaging tests, such as a CT scan or MRI, to help with surgical planning
How Is Tetralogy of Fallot (TOF) Treated?
Doctors repair tetralogy of Fallot through open-heart surgery soon after birth or later in infancy, depending on the baby's health and weight and severity of defects and symptoms.
The two surgical options are:
- Complete repair: The surgeon widens the passageway between the right ventricle and the pulmonary artery to improve blood flow to the lungs. The ventricular septal defect is patched to stop the mixing of high-oxygen blood with low-oxygen blood between the ventricles.
These repairs also fix the two remaining defects (overriding aorta and right ventricular hypertrophy). Because the right ventricle doesn't have to work as hard to pump blood into the lungs, the thickness of the ventricle wall will decrease. And the patched VSD prevents blood with low oxygen from flowing into the aorta. - Temporary or palliative surgery: Minor repairs can improve blood flow to the lungs. This usually is done only when a baby is too weak or small to have full surgery. The surgeon creates a secondary route for blood to travel to the lungs for oxygen by placing a small tube (called a shunt) between a large artery branching off the aorta and the pulmonary artery.
The full repair is done later when the baby grows stronger.
Most babies whose tetralogy of Fallot is repaired do very well. After surgery, they will need regular follow-up visits with a heart specialist, even as adults.

© 1995- The Nemours Foundation. KidsHealth® is a registered trademark of The Nemours Foundation. All rights reserved.
Images sourced by The Nemours Foundation and Getty Images.