- Home
- Parents Home
- Allergy Center
- Asthma Center
- Cancer Center
- Diabetes Center
- A to Z Dictionary
- Emotions & Behavior
- First Aid & Safety
- Food Allergy Center
- General Health
- Growth & Development
- Flu Center
- Heart Health
- Homework Help Center
- Infections
- Diseases & Conditions
- Nutrition & Fitness Center
- Play & Learn Center
- School & Family Life
- Pregnancy Center
- Newborn Center
- Q&A
- Recipes
- Sports Medicine Center
- Doctors & Hospitals
- Videos
- Para Padres
- Home
- Kids Home
- Asthma Center
- Cancer Center
- Movies & More
- Diabetes Center
- Getting Help
- Feelings
- Puberty & Growing Up
- Health Problems of Grown-Ups
- Health Problems
- Homework Center
- How the Body Works
- Illnesses & Injuries
- Nutrition & Fitness Center
- Recipes & Cooking
- Staying Healthy
- Stay Safe Center
- Relax & Unwind Center
- Q&A
- Heart Center
- Videos
- Staying Safe
- Kids' Medical Dictionary
- Para Niños
- Home
- Teens Home
- Asthma Center
- Be Your Best Self Center
- Cancer Center
- Diabetes Center
- Diseases & Conditions
- Drugs & Alcohol
- Expert Answers (Q&A)
- Flu Center
- Homework Help Center
- Infections
- Managing Your Medical Care
- Managing Your Weight
- Nutrition & Fitness Center
- Recipes
- Safety & First Aid
- School & Work
- Sexual Health
- Sports Center
- Stress & Coping Center
- Videos
- Your Body
- Your Mind
- Para Adolescentes
Pancreatitis
What Is Pancreatitis?
Pancreatitis is an of the pancreas. It can cause symptoms like those of a stomach virus, like belly pain, vomiting, and nausea.
In most cases, pancreatitis gets better on its own.
What Are the Types of Pancreatitis?
Pancreatitis can be:
- acute and last for only a few days. This is more common in kids and most kids have only one episode.
- chronic and last for a long time. This ongoing inflammation can permanently damage the pancreas.
What Are the Signs & Symptoms of Pancreatitis?
Kids with pancreatitis usually have sudden, severe pain in the upper belly. They also might have pain in the back, chest, or sides.
Other pancreatitis signs include:
Children with chronic pancreatitis may also have:
- diarrhea
- greasy poop that is hard to flush
- weight loss and poor growth
- poor blood sugar control (high blood sugar or low blood sugar)
Some kids who have repeated episodes of acute pancreatitis can develop chronic pancreatitis.
What Does the Pancreas Do?
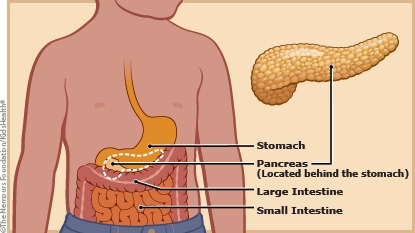
The pancreas is a large gland that sits behind the stomach. It makes digestive enzymes that are released into the small intestine to help break down food. The pancreas also makes insulin and glucagon, two hormones that help control blood sugar levels.
What Causes Pancreatitis?
Common causes of pancreatitis in kids include:
- gallstones or problems with the ducts (tubes) in the pancreas or liver
- infections
- some medicines
- traumatic injury to abdomen
- very high triglycerides
- genetic or inherited disorders
Some medical conditions or illnesses, such as cystic fibrosis or celiac disease, can increase a child's risk for pancreatitis. Sometimes, the cause of pancreatitis isn't found.
How Is Pancreatitis Diagnosed?
To diagnose pancreatitis, doctors will order blood tests, including tests that measure the pancreatic enzymes amylase and lipase. If these levels are high, an abdominal ultrasound can help the doctor check the liver and pancreas and look for gallstones.
Other tests, such as a CAT scan or MRI, can check for inflammation or damage to the pancreas.
How Is Pancreatitis Treated?
Most of the time, pancreatitis gets better on its own in about a week. As the pancreas heals, doctors can give medicine to control pain and treat nausea and vomiting.
Kids who can drink enough fluids and whose pain eases with oral pain medicine can be cared for at home. Children with more severe pancreatitis will need care in the hospital. They'll get intravenous (IV) fluids and pain medicine. The care team will watch for complications, such as infection, breathing problems, or kidney problems.
Doctors recommend that kids with mild pancreatitis start eating as soon as possible. Kids with more serious cases may get formula through a feeding tube that goes right into the stomach or small intestine. Some might need to get IV nutrition — called total parenteral nutrition (TPN).
Some children with pancreatitis need a procedure called endoscopic retrograde cholangiopancreatography (ERCP). ERCP lets doctors see the ducts in the pancreas and liver. During the ERCP, doctors can remove gallstones or find and treat other causes of pancreatitis.
What Else Should I Know?
Most children with acute pancreatitis recover without any problems. Fluid in and around the pancreas can happen, but usually gets better on its own. Sometimes, doctors need to drain the fluid.
Kids with chronic pancreatitis have trouble digesting food and usually need to take pancreatic enzyme supplements. Chronic pancreatitis may lead to diabetes, but this usually takes many years to happen.

© 1995- The Nemours Foundation. KidsHealth® is a registered trademark of The Nemours Foundation. All rights reserved.
Images sourced by The Nemours Foundation and Getty Images.