Arteriovenous Malformations
What Is an Arteriovenous Malformation (AVM)?
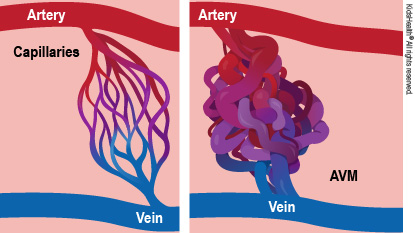
An arteriovenous malformation (AVM) is the result of one or more abnormal connections between an artery (a blood vessel carrying blood from the heart out to the body) and a vein (a vessel returning blood to the heart).
It's a shortcut that lets blood flow from an artery to a vein without passing through tiny vessels called capillaries. That's important because oxygen and other nutrients can only pass from the blood into the body's organ through the capillaries.
Any blood that takes a shortcut through an AVM returns oxygen-rich blood to the heart instead of delivering it to the body. That means some of the heart's work is wasted, so the heart has to work harder than usual. Large AVMs or multiple AVMs can waste so much of the heart's work that it cannot keep up.
What Are the Signs & Symptoms of an Arteriovenous Malformation (AVM)?
A child with an arteriovenous (ar-teer-ee-oh-VEEN-is) malformation may have these signs:
- a pink, red, or purple birthmark
- pain
- swelling
- bleeding, which may be hard to stop
- warmer skin over the AVM
- a pulse that's felt around the AVM
Many AVMs, especially those in the head, are not recognized until adulthood. AVMs in the head may cause:
- headaches
- trouble with body movements or speech
- loss of strength or sensation
- seizures
- vision problems
- confusion
- problems understanding speech
Bleeding from an AVM can be hard to stop. Frequent bleeding may lead to anemia (a low number of red blood cells). Even small amounts of bleeding inside the skull can be very dangerous. AVMs may grow larger and cause trouble by pressing on other parts of the body.
What Causes Arteriovenous Malformations?
Arteriovenous malformations are a type of vascular malformation (also called vascular anomalies) that happen when blood vessels do not develop normally.
Doctors don't know what causes AVMs. Kids who have them are born with them, and an AVM might get larger as the child grows.
AVMs can happen with some genetic syndromes, including:
- Cobb syndrome: vascular malformations of the skin, including wine-colored birthmarks, and AVMs in the spine, spinal canal, and/or spinal cord
- hereditary hemorrhagic telangiectasia (HHT): AVMs in the lungs, brain, and digestive tract
- Parkes Weber syndrome: multiple AVMs in one arm or leg; the affected arm or leg typically grows longer and larger than the same limb on the other side
- Wyburn-Mason syndrome (also known as Bonnet-Dechaume-Blanc syndrome): AVMs of the retina (the light-sensitive area in the back of the eye) and brain, sometimes involving part of the face
How Is an Arteriovenous Malformation Diagnosed?
Doctors often find an AVM during an exam because they can feel a pulse in its vessels. Then, they use other tools to learn more about it and plan treatment, such as:
- an ultrasound, to determine the pattern of blood flow through the AVM
- a CT scan or MRI, to see the AVM's size and how close it is to normal body parts
- an angiogram, to map the AVM's blood vessels, which will help doctors plan how to block blood flow to it
- an MRA, or MRA angiogram, which uses special MRI techniques to map the AVM without using X-rays. In some cases, a CT angiogram can help them diagnose the AVM.
- a standard angiogram, which uses live X-rays to map the AVM's blood vessels. This can help doctors plan how to decrease or block blood flow through the AVM.
How Is an Arteriovenous Malformation Treated?
How doctors treat an arteriovenous malformation depends on its location and size, and how it affects the child. AVMs in the arms, legs, and body are easier to treat than those in the head.
Doctors may treat an AVM to:
- ease pain
- reduce bleeding
- make it smaller and/or lessen its effects on nearby organs
When a child's heart works harder than usual because of an AVM, quick treatment helps prevent long-term changes to the heart's muscle or possible heart failure.
AVMs that are not in the skull are treated with:
- embolization: a catheter (thin, flexible tube) permanently blocks the arteries feeding the AVM with synthetic materials
- sclerotherapy: injection of a medicine or medical-grade substance into an AVM that shrinks the blood vessels
- surgery
AVMs in the head are called intracranial AVMs. Doctors may treat these with embolization, surgery alone, or surgery with radiation (radiosurgery).
Interventional radiologists, doctors who specialize in minimally invasive image-guided procedures, usually do the embolization and sclerotherapy treatments.
What Else Should I Know?
How doctors treat an AVM depends on its size, where it is, and what symptoms it causes. A small AVM that's not in the head may never need treatment, but could change as a child grows. Some arteriovenous malformations get bigger, so it's important to track their size and effects on a child's health and activities.
Kids may feel shy or embarrassed about how an arteriovenous malformation looks. Be sure to support your child emotionally. It can help to find a local support group where other families can talk about what works for them. Ask your child's care team about it. You also can look online at:
Talking to a therapist can help kids and teens if they're feeling sad or upset about an arteriovenous malformation or its treatment.


